Chest Infections: What Patients Mean vs. What Clinicians Diagnose
- Global Guest

- Jul 20, 2025
- 6 min read
By Global Health Pneumology Insights

When many people say they have a “chest infection,” they’re describing a mix of symptoms—cough, mucus, chest tightness, maybe fever—that feel like “something on the chest.” But in medicine, “chest infection” isn’t a precise diagnosis. It’s a lay term that may refer to several different conditions affecting the airways, lung tissue, or even the lining around the lungs. Understanding the difference matters because the cause, severity, and treatment can vary widely.
In this article, we’ll clarify what “chest infection” usually means, review the most common clinical conditions it may refer to, outline symptoms and causes, and explain when to seek medical care.
Quick Takeaways
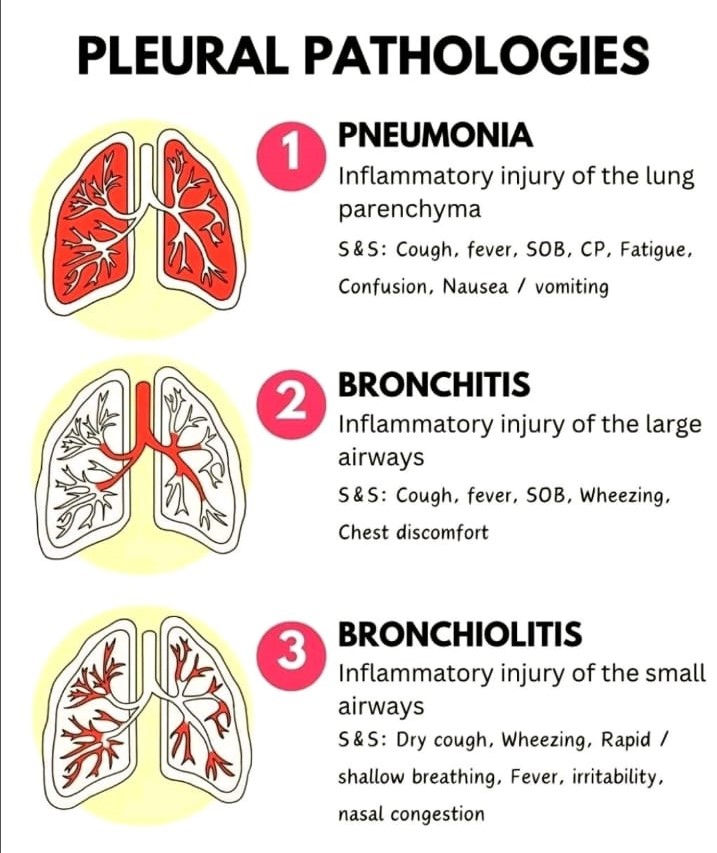
“Chest infection” is not a medical diagnosis. It can refer to bronchitis, pneumonia, bronchiolitis (in children), or flare-ups of chronic lung disease.
Not all chest infections need antibiotics—most are viral.
Red flag symptoms (shortness of breath, high fever, confusion, chest pain, low oxygen) need same‑day medical review.
Vaccination, hand hygiene, smoking cessation, and good chronic disease control reduce risk.
What People Often Mean by “Chest Infection”
Common patient descriptions include:
“My cold has moved to my chest.”
“I’m coughing stuff up.”
“I feel rattly when I breathe.”
“I’ve tightness in my chest with a cough.”
These experiences are real—but they don’t tell us which structure in the respiratory system is inflamed. That distinction guides treatment.
What Clinicians Consider When Hearing “Chest Infection”
Lay Term: “Chest Infection” | Possible Clinical Condition | Main Area Affected | Typical Cause | Antibiotics? |
Bad cough with mucus after a cold | Acute Bronchitis | Large airways (bronchi) | Usually viral | Usually no |
Fever + productive cough + shortness of breath | Pneumonia | Lung parenchyma (air sacs) | Bacterial, viral | Often yes (if bacterial) |
Wheezy infant with fast breathing | Bronchiolitis | Small airways (bronchioles) | Viral (RSV common) | No (supportive) |
Sharp pain with deep breath + fever | Pleurisy / Pleuritis ± effusion | Pleura (lining of lung) | Viral, bacterial, other | Depends on cause |
Chronic cough in smoker, recurring mucus | Chronic Bronchitis / COPD flare | Airways | Smoking-related; infections trigger flares | Sometimes |
“Chest congestion” but no fever, mainly upper throat | Upper Respiratory Infection (not chest) | Nose/throat | Viral | No |
Anatomy Refresher: Where Can Infection Occur?
The respiratory tract has several levels:
Upper airway: nose, throat, sinuses.
Large lower airways: trachea → bronchi.
Small airways: bronchioles.
Alveoli / Lung parenchyma: where oxygen exchange happens.
Pleura: thin lining around lungs and chest wall.
Symptoms vary depending on which level is affected.
Common Chest Infections & How They Present
1. Acute Bronchitis
What it is: Inflammation of the large airways (bronchi), usually after a viral cold.
Key Symptoms:
Persistent cough (may last 2–3+ weeks)
Mucus / phlegm production (clear → yellow/green; colour alone does not prove bacteria)
Chest tightness or “rattling”
Mild fever or none
Wheeze in some patients
Causes: Mostly viral (influenza, RSV, rhinovirus, coronavirus strains). Less commonly bacterial.
Treatment:
Symptom relief: fluids, rest, humidified air.
Cough suppressants or expectorants when appropriate.
Inhaled bronchodilators if wheezy (particularly in people with asthma/COPD).
Antibiotics rarely needed unless bacterial infection suspected or high‑risk patient.
When to see a doctor: Fever >38°C, breathlessness, cough >3 weeks, underlying lung disease, or if unsure.
2. Pneumonia
What it is: Infection of the lung tissue (parenchyma)—the air sacs fill with inflammatory fluid, reducing oxygen exchange.
Key Symptoms:
Fever, chills
Productive cough (but elderly may have dry cough)
Shortness of breath
Chest pain worse with breathing or coughing
Fatigue, weakness
Confusion (especially in older adults)
Nausea / vomiting sometimes
Causes:
Bacterial: Streptococcus pneumoniae, Haemophilus influenzae, atypicals (Mycoplasma, Chlamydophila), Staph aureus.
Viral: Influenza, SARS‑CoV‑2, RSV (esp. infants/older adults).
Aspiration: Inhaling food/liquids into lungs.
Diagnosis: Exam, oxygen check, chest X‑ray, sometimes blood tests, sputum culture.
Treatment:
Antibiotics for bacterial pneumonia (choice depends on severity & risk factors).
Antivirals in selected viral infections (e.g., flu antivirals if early).
Oxygen, fluids, fever control.
Hospitalization for moderate to severe cases (low oxygen, advanced age, co‑morbidities).
Prevention: Pneumococcal and flu vaccines are highly protective in at‑risk groups.
3. Bronchiolitis (Mostly in Infants & Young Children)
What it is: Viral inflammation of the smallest airways (bronchioles) causing swelling and mucus plugging.
Key Symptoms:
Runny nose followed by dry or wet cough
Wheezing or crackly breathing
Rapid / shallow breathing, chest retractions in severe cases
Poor feeding, irritability
Fever (not always high)
Causes: Respiratory Syncytial Virus (RSV) is the leading cause; also rhinovirus, influenza, parainfluenza, adenovirus.
Treatment:
Mostly supportive: fluids, nasal suctioning, monitoring breathing.
Oxygen if saturation low.
Hospital care for infants with breathing difficulties, dehydration, or high risk (premature, heart/lung disease).
Routine antibiotics are not used (viral cause).
Prevention: Hand hygiene, avoiding exposure during RSV season, and RSV preventive monoclonal antibodies for high‑risk infants where available.
4. Pleurisy / Pleural Infection (Parapneumonic Effusion, Empyema)
What it is: Inflammation or infection of the pleura—the double membrane around the lungs. Sometimes fluid collects (pleural effusion); if pus, it’s called empyema.
Key Symptoms:
Sharp, stabbing chest pain worse on deep breath or cough
Shortness of breath (if fluid builds up)
Fever (if infected)
Dry cough
Causes: Often secondary to pneumonia; also viral infections, autoimmune disease, pulmonary embolism, or post‑surgery.
Diagnosis: Exam, chest X‑ray, ultrasound, sometimes CT. Thoracentesis (needle sample) if fluid.
Treatment:
Treat underlying cause (e.g., antibiotics for bacterial pneumonia).
Drainage of fluid or pus if large or infected.
Pain control is essential (NSAIDs, as clinically appropriate).
5. COPD Exacerbation / Chronic Bronchitis Flare
Some patients who say “I’ve another chest infection” actually have a flare of chronic lung disease, commonly COPD.
Key Symptoms:
Increased cough & sputum volume
Change in sputum colour (not always infection)
Worsening breathlessness
Wheeze
Triggers: Viral infections, air pollution, cold weather, bacterial infection, missed inhalers.
Treatment:
Step‑up inhaled bronchodilators
Oral corticosteroids for moderate/severe exacerbations
Targeted antibiotics if increased sputum purulence, volume, and breathlessness (per guidelines)
Oxygen if needed; sometimes non‑invasive ventilation in severe cases.
Symptom Guide: When Is It More Than a Simple Viral Bug?
Symptom | Likely Minor / Viral | See GP Soon | Seek Urgent / Emergency Care |
Fever | Low‑grade <38°C | Persistent >3 days | >39°C + breathlessness/confusion |
Cough | Mild, dry | Productive, lasting >3 wks | Blood in sputum, severe distress |
Breathing | Normal at rest | Mild shortness of breath | Struggling to breathe, blue lips |
Chest Pain | None / mild tightness | Discomfort with cough | Sharp pain on breathing, severe pain |
Mental Status | Normal | Very fatigued | Confusion, drowsiness |
Causes & Risk Factors for Chest Infections
Infectious Agents:
Viruses (most common overall)
Bacteria
Fungi (rare; immunocompromised)
Aspiration of food/liquids (especially in elderly or swallowing disorders)
Risk Factors:
Age <2 or >65
Chronic lung disease (asthma, COPD, cystic fibrosis)
Smoking
Immune suppression (medications, HIV, cancer therapy)
Diabetes, heart disease
Poor vaccination status
Crowded living conditions or healthcare exposure
Diagnosis: What Your Clinician May Do
History & exam – symptom duration, fever, exposure, medical history.
Listen to lungs – crackles, wheeze, reduced breath sounds, pleural rub.
Vitals & oxygen saturation – important for triage.
Tests (as needed):
Chest X‑ray (pneumonia? effusion?)
Blood tests (infection markers)
Sputum culture (selected cases)
Viral swabs (flu, RSV, COVID‑19)
Arterial blood gas for severe illness
Not every cough needs a chest X‑ray—your provider will guide you.
Treatment Overview by Condition
Condition | Main Treatment | Do Antibiotics Help? | Home vs. Hospital |
Acute Viral Bronchitis | Fluids, rest, cough relief, inhalers if wheezy | No | Home |
Bacterial Pneumonia | Targeted antibiotics, supportive care | Yes | Depends on severity |
Viral Pneumonia | Supportive; antivirals for some viruses | Usually no (unless bacterial superinfection) | Mild: Home; Severe: Hospital |
Bronchiolitis (infants) | Supportive, oxygen if needed | No | Many home; severe to hospital |
Pleurisy/Empyema | Treat cause, drain fluid, pain relief | Yes if bacterial | Often hospital if significant |
COPD Flare | Inhalers, steroids, +/- antibiotics | Sometimes | Varies |
Self‑Care Tips (Mild Illness Only)
Always seek medical advice if unsure or if symptoms worsen.
Stay hydrated to help thin mucus.
Use over‑the‑counter fever reducers if safe for you (e.g., paracetamol/acetaminophen).
Honey (for adults & >1 year old children) can reduce cough frequency.
Humidified air or steamy showers may ease congestion.
Avoid smoking and second‑hand smoke.
Prevention: Protect Your Lungs
Vaccines: Influenza, pneumococcal, COVID‑19, pertussis (Tdap), RSV protection for high‑risk infants.
Stop smoking: One of the strongest ways to prevent chronic lung disease and recurrent infections.
Hand hygiene: Especially during cold/flu season.
Masking when ill or exposed: Reduces spread of respiratory viruses.
Manage chronic conditions: Good asthma/COPD control lowers risk of severe infection.
When to Contact Global Health
Reach out to us if you or a family member has:
Fever with cough lasting more than a few days
Worsening shortness of breath
Chest pain when breathing
A child breathing fast, feeding poorly, or wheezing
Repeated “chest infections” (you may need further evaluation)
Our multidisciplinary team can assess symptoms, arrange testing, prescribe treatment when needed, and help you prevent future infections.
.



Comments